Having a baby is an exciting and special time, but labor can be painful. And it's important that you be well-informed about your options for pain control.
You have many choices for pain relief during labor, which include unmedicated methods such as breathing techniques or massage, and medicated options such as IV pain medication, breathing in nitrous oxide, or getting an epidural. The decision is personal, and you may choose a combination of methods.
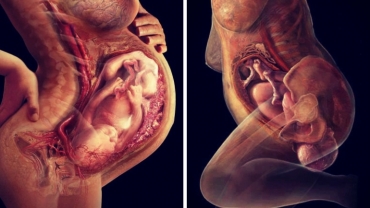
An epidural involves putting a local anesthetic or numbing medication like what you get when you go to the dentist into the epidural space in your back. The epidural will deliver a continuous infusion of medicine that works directly on the nerves in your back and numbs the lower half of your body in contrast to systemic medications, which act on your brain and sedate you.
An epidural acts locally at the nerves that transmit pain from the uterus and the vagina. And since the epidural medicine works directly on the nerves in your back, very little medicine gets to your baby; and you can safely breastfeed after having an epidural. You can get an epidural at any time once you've gone into labor.
Typically it'll take about 30 minutes to get the epidural catheter started, and then an additional 15 minutes or so for the medicine to work. If you have obesity or scoliosis, it may take slightly longer.
We're not actually gonna place the catheter today because the patient here is not quite at that stage, but so what we would do at this point is put a little numbing medication here in the skin. One thing that's really helpful is the positioning of the spine here, and what we're trying to get is a curve right down at the base.
So, Christina, if you can just, yeah, curve over the baby like an angry cat, and then curve, push once against me here. That's beautiful. So the curve, this is the area that we're trying to get the curve into to help separate the bones of the spine to make the gap bigger for the catheter to go in. Okay.
And then we use another needle to help get this thin, floppy catheter into place to drip medication right next to the nerves coming out of the spine.
During this part you should only feel pressure, sometimes a needle or a catheter may brush against the nerve and cause a brief electric feeling similar to when you bang your funny bone, but nothing more serious than that.
Once the catheter's in place, we then secure it with some tape, up the back, and over the shoulder where we can connect it to the medication. The soft catheter will then stay in your back until you deliver your baby with a constant infusion of medication.
The epidural can also stay in place and be used in the event that you need a Cesarean section. You can expect to slowly feel your contractions becoming less intense and shorter, and your legs may feel weak and heavy like they've fallen asleep.
You'll also have your nurse place a catheter into your bladder after you've had your epidural. And many studies have shown that an epidural does not significantly slow down labor, and if it does, it only increases the second stage of labor by a few minutes.
And there's no evidence that epidurals increase the likelihood of needing a Cesarean section. Sometimes the epidural needs some fine tuning, and one in every 10 women will need the epidural replaced.
Even with the epidural, you should expect to feel pelvic pressure, especially when the baby's head is low, and you're about to deliver.
And the ability to feel pressure is good 'cause it lets you know when it's time to push. An epidural might decrease your blood pressure, which might cause you to have nausea and vomiting, so you'll be given IV fluids to try and prevent this.
And your anesthesiologist will watch your blood pressure closely after you receive the epidural, provide treatments if necessary. You could develop a fever, or itchiness, shivering, or experience temporary soreness at the epidural site, which may last for several days.
But general back pain is not caused by epidurals though it's common after any delivery. Rarely, around one in a hundred or 1% of women will develop a severe headache called a post-dural puncture headache, which can last for several days if not treated.
Serious complications after an epidural, such as the misplacement of the catheter into a vein, potentially causing seizures, is very rare. A block at a higher level than intended, requiring intubation and breathing assistance, again, very rare.
Serious nerve injury: one in 20,000 to one in 200,000.
Bleeding: one in 40,000 to one in a million.
Infection: one in 20,000 to one in 200,000. Or other life-threatening complications are exceedingly rare.
Staying comfortable is an important part of a positive birthing experience. Your anesthesiologist is a pain-management specialist who works with your obstetrician to help you safely through the birthing process.
Feel free to discuss all your options for pain control during delivery with your obstetrician and anesthesiologist so that you can make an informed decision.
- 1898 views