Having diabetes, any type of diabetes, means that you have too much glucose, a form of sugar, in your bloodstream. When you have gestational diabetes, your blood glucose has risen above normal during your pregnancy. Gestational diabetes may occur anytime during your pregnancy.
Women are more likely to develop gestational diabetes if they are: 25 years or older at their first pregnancy, were overweight before they became pregnant, have a family history of diabetes, or have already had a baby that weighed more than nine pounds at birth. Being of African American, Pacific Island, Hispanic, or Native American descent also increases your risk. But gestational diabetes can also occur in pregnant women who have no risk factors.
Diabetes affects the way your body uses the food you eat. To understand gestational diabetes, it helps to understand how your body changes food into energy.
Most of the food you eat changes to glucose, a form of sugar. Glucose enters the bloodstream, causing your blood glucose level to rise. As your blood glucose rises, the pancreas releases insulin. Insulin works like a key to open the cells and let glucose enter. The glucose is used for energy immediately or stored for later use.
Because this process removes the glucose from your bloodstream, insulin helps your blood glucose level to stay in a healthy range.
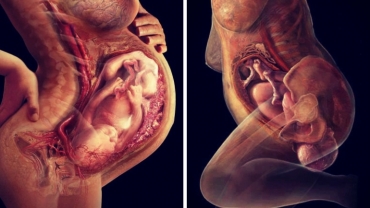
Your blood vessels also supply your baby with energy. They carry glucose, oxygen, and other nutrients to your baby through an organ called the placenta. At the same time your placenta is passing nutrients to your baby, it releases hormones into your bloodstream that support a healthy pregnancy.
As your baby and placenta grow and develop, more hormones are produced. By the sixth through ninth months of pregnancy, this increase in hormones can cause your cells to stop letting insulin do its job. This is called insulin resistance. This is why most women are tested for gestational diabetes between weeks 24 and 28.
In order to balance the insulin resistance, the pancreas needs to produce more and more insulin to move glucose out of the bloodstream and into the cells for energy now or for later use. In fact, the amount of insulin you need may increase by 2–3 times during pregnancy.
Most women produce enough extra insulin to keep their blood glucose level in a healthy range. But if your cells resist the insulin, they cannot open up to let the glucose in. Glucose stays in your bloodstream leading to high blood glucose, or hyperglycemia. This is called diabetes.
Meet with your healthcare provider as soon as you find out you have gestational diabetes to set up your management plan. You’ll learn the steps you need to take to lower your blood glucose for your healthy pregnancy and healthy baby.
- 5131 views